Last month, news outlets around the world heralded what could be a major medical breakthrough. In the midst of a public health battle against antibiotic resistant germs — which have been popping up with alarming frequency, not just in hospitals but in sick household pets and in meat from the supermarket — researchers announced the discovery of a powerful new antibiotic. Teixobactin easily cured mice of pneumonia and MRSA (an antibiotic resistant staph infection), and is likely to be effective against other deadly diseases such as anthrax. Yet this promising antibiotic has humble beginnings. It is produced by a soil bacterium discovered in a sample of dirt taken from a Maine field. Turning an evolutionary lens on this story reveals the explanation for teixobactin’s power and suggests that more new antibiotics might be literally in our own backyards.
Where's the evolution?
Most of the antibiotics in use today are produced by microorganisms like bacteria. Evolutionary history explains why comparatively simple organisms can make such sophisticated compounds. As they compete for resources, bacteria are fighting a war against each other. Over many generations, some bacterial lineages evolved ways of attacking other bacteria. In response, the defenders with stronger protections were favored, and the assailants, in turn, evolved even better weapons, and so on. This arms race has been playing out over four billion years of bacterial evolutionary history, so the combatants have had plenty of time for natural selection to fine tune their weaponry. Antibiotics like vancomycin and teixobactin are the munitions that certain bacteria species have evolved over the course of this ongoing fight. We humans have simply coopted these highly evolved compounds and put them to work against the bacteria that attack us.
The discovery of antibiotics in 1929 and their subsequent mass production ushered in a new era in medicine. Antibiotics could cure diseases that were previously untreatable and contributed to major reductions in infectious disease deaths throughout the world. During the golden age of antibiotic discovery in the 1950s, half of the antibiotics that we depend on today were found by screening microorganisms — many of them soil bacteria — for antibacterial properties that they’d evolved to combat one another. But the promise of these discoveries would soon dim. Most antibiotics have short shelf lives. In general, once an antibiotic becomes widely prescribed, resistant bacterial strains evolve within a few years — a continuation of that age old arms race in modern medical setting. Since the 1960s, antibiotic resistant bacteria have been on the rise. Today the situation is dire. Common diseases like urinary tract infections now frequently appear as drug-resistant forms, multi-drug resistant tuberculosis is widespread, and some hospital-based infections can no longer be effectively treated with any existing antibiotic.
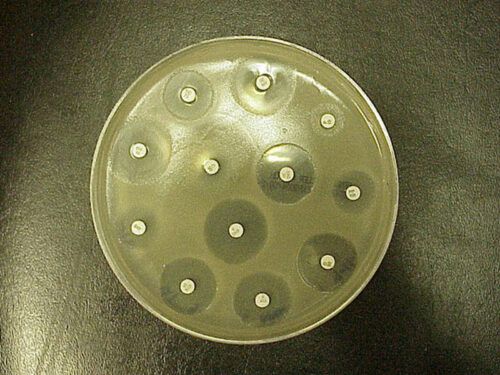
We need new drugs, but during the 1950s, we discovered most of the antibiotics being produced by easy-to-cultivate bacteria, plucking all the low hanging fruit from the tree of life. Since then, new antibiotics have only rarely surfaced. The discovery of teixobactin is particularly hopeful because it was found using a novel method for cultivating soil bacteria that involves first culturing the bacteria in their native dirt. This technique will allow researchers to screen for new drugs more easily.
The bacteria that produce teixobactin (Eleftheria terrae) were first identified in this screening because they killed staph bacteria. Further studies revealed that teixobactin worked against any Gram-positive pathogen (that is, bacteria with a thick layer of sugars and amino acids, known as peptidoglycan, in their cell walls). Gram-positive bacteria include tuberculosis, anthrax, listeria, and plenty of other nasty bugs. Perhaps even more exciting, the new molecule was effective against drug resistant strains. And when the researchers tried to set up conditions that would encourage bacteria to evolve resistance to teixobactin, none did. These useful properties of the antibiotic also have an evolutionary explanation, but in this case, one that has to do with how bacteria evolve resistance.
Many antibiotics work by attacking a protein that bacteria need to survive. Penicillin, for example, ties up a protein that bacteria use to build and upkeep their cell walls, causing the cell to die. However, that wall-building protein is encoded directly in the bacterial DNA, and any mutations that affect that gene could change the protein in a way that prevents penicillin from binding to it, generating a penicillin-resistant bacteria strain. Teixobactin, on the other hand, works by binding to one of the building blocks of peptidoglycan itself, which is not a protein and, hence, is not directly encoded in DNA. Instead, this peptidoglycan precursor is produced by chemical reactions within the cell. While evolving resistance to penicillin might require just one or a few changes to a single gene, evolving resistance to teixobactin would require more of an evolutionary leap since there is no single gene that codes for production of peptidoglycan.
The researchers behind this discovery hypothesize that it might not even be possible for a series of mutations to change the chemical synthesis of peptidoglycan in a way that shields it from teixobactin. Instead they suspect that if resistance to teixobactin evolves, it would probably come in the form of a gene that codes for a protein that deactivates the drug. The antibiotic vancomycin works in a similar way to teixobactin, and it took 30 years for resistance to vancomycin to arise. Scientists expect that it will take even longer for teixobactin-resistant strains to evolve.
Of course, the day that a patient can receive a teixobactin injection to treat a case of extensively drug resistant tuberculosis is still several years off — if it comes at all. Before the new drug reaches hospitals or doctors’ offices, it needs more testing to establish that it is effective and safe for humans. Nevertheless, there is plenty of reason to hope that teixobactin will soon be used to fight some of the toughest antibiotic resistant infections that patients now face — and that it will merely be the first in a series of drugs that the new culturing technique allows us to discover. Perhaps, more fully exploring the diverse chemicals that billions of years of natural selection have produced will open the doors to a new “golden age” of antibiotic discovery.
Primary literature:
- Davies, J., and Davies, D. (2010). Origins and evolution of antibiotic resistance. Microbiology and Molecular Biology Reviews. 74: 417-433. Read it »
- Ling, L. L., Schneider, T., Peoples, A. J., Spoering, A. L., Engels, I., Conlon, B. P., ...Lewis, K. (2015). A new antibiotic kills pathogens without detectable resistance. Nature. doi: 10.1038/nature14098 Read it »
News articles:
- A summary of the discovery from the New York Times
- A thorough review of the research with an evolutionary angle from the blog Not Exactly Rocket Science
Understanding Evolution resources:
-
- In your own words, explain what happens during an evolutionary arms race.
- Do some research online to find another example of an evolutionary arms race that does not involve bacteria and resistance to antibiotics. Describe that example.
- Review the concept of evolutionary fitness. Would teixobactin increase the fitness of a bacterium that produced it relative to a lineage that did not produce it? Explain your reasoning.
- Review the process of natural selection. Use the four steps described on that page to explain how a bacterial lineage might evolve resistance to penicillin.
- Advanced: Why is it significant in terms of the evolution of resistance that teixobactin works by attacking a molecule that is not a bacterial protein?
- Advanced: Review the concept of adaptation. Is teixobactin an adaptation for E. terrae or do you have enough information to say? Explain your reasoning.
- Teach about the evolution of resistance bacteria: In this lesson for grades 9-16, students learn why evolution is at the heart of a world health threat by investigating the increasing problem of antibiotic resistance in such menacing diseases as tuberculosis.
- Teach about evolutionary arms races: In this case study for grades 9-16, students find out how an evolutionary arms race has pushed the rough-skinned newt to the extremes of toxicity and how evolutionary biologists have unraveled their fascinating story.
- Davies, J. (2006). Where have all the antibiotics gone? The Canadian Journal of Infectious Diseases and Medical Microbiology. 17: 287-290.
- Davies, J., and Davies, D. (2010). Origins and evolution of antibiotic resistance. Microbiology and Molecular Biology Reviews. 74: 417-433.
- Ling, L. L., Schneider, T., Peoples, A. J., Spoering, A. L., Engels, I., Conlon, B. P., ... Lewis, K. (2015). A new antibiotic kills pathogens without detectable resistance. Nature. doi: 10.1038/nature14098
- World Health Organization. (2014). Antimicrobial resistance: global report on surveillance. Retrieved January20, 2014 from the World Health Organization