Amidst and following growth in vaccine hesitancy, measles cases are on the rise again in the United States. A recent outbreak in Texas and New Mexico so far involves more than 140 cases, the majority among children and youth, and has caused the death of a child. One of the most contagious human diseases known, measles travels easily through the air, remains alive on surfaces for hours, and can be transmitted for many days before it causes symptoms. Someone with measles will infect 90% of the unprotected people with whom they come into contact, leading to explosive outbreaks if vaccination rates are low. So even though measles is only occasionally deadly – around 2 of every 1000 children infected will die from complications, a small but significant risk – outbreaks can be massive and cause many deaths, especially among the most vulnerable. An outbreak in 2018 killed 140,000 people around the world, mostly children under five. The bright spot here is that the two doses of the MMR (measles, mumps, and rubella) vaccine are safe and very effective at preventing both illness and transmission for life. Why is the MMR vaccine so steadfast, when our COVID and flu shots need regular updates? The answer is, of course, evolution…
Where's the evolution?
Measles is an RNA virus, meaning that its genome is encoded in single-stranded RNA instead of the double-stranded DNA molecule. Other RNA viruses include HIV, influenza, and SARS-CoV-2, the virus behind COVID-19. RNA viruses have high mutation rates, as discussed in a recent news story on bird flu. DNA is a stable molecule, with two copies of the information it encodes, one in each strand of the double helix. RNA, on the other hand, is less stable and has no back-up copy of its data, leading to more mutations – mistakes in repair or copying – compared to DNA. High mutation rates, in turn, increase the amount of genetic variation in a population, making it more likely that an advantageous variant will arise (or already exist!) and sweep through the population via natural selection.
Partly because of their RNA genomes and high mutation rates, the HIV, influenza, and SARS-CoV-2 viruses evolve quickly, presenting a challenge to vaccine development. Vaccines work by “teaching” our bodies to recognize and fight a particular pathogen. But these three viruses rapidly evolve traits that make them unrecognizable to an immune system primed to recognize a prior version of a virus. In the case of influenza, the World Health Organization constantly monitors the evolution of different viral strains in order to anticipate which strains are likely to dominate in upcoming flu seasons and to redesign the yearly flu vaccine accordingly. COVID vaccines also need regular updates to keep up with viral evolution. And HIV’s high rate of evolution is one of the reasons that scientists have not yet managed to develop an effective HIV vaccine.
In contrast, the measles vaccines available in the U.S. are based upon a viral strain collected from a single patient in 1954, and they work against all strains of measles that have evolved since. The measles vaccine introduced in the 1960s remains just as effective today as it was then. Why do other RNA-based viruses like influenza and SARS-CoV-2 evolve out from under our vaccines, while the measles virus remains vulnerable to the same old vaccine we’ve used for 50+ years? Research reported in 2021 suggests that the answer has to do with constraints on the evolution of the measles virus.
To understand, you first need to know a little about how the measles vaccine and immunity work. The measles vaccine is simply a strain of the virus developed to carry mutations that make it weak and unable to cause illness. When we are vaccinated, the weakened virus multiplies within us, and our immune systems respond to it, producing a variety of antibodies that bind to different parts of two proteins on the surface of the virus: the H and F proteins (short for hemagglutinin and fusion). These bound antibodies mark the virus for destruction. Importantly, in this process, the immune system also gains the ability to produce anti-measles antibodies quickly in the future, so that the next time it encounters the measles virus – for example, through exposure to the wild, unweakened virus – it can respond right away and destroy the virus before it can sicken us or be passed on to someone else.
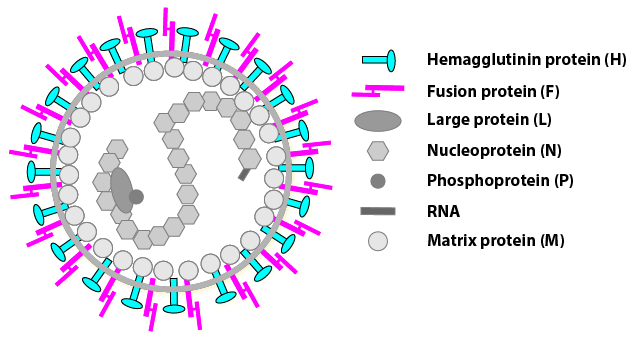
Research into why the measles vaccine has remained so effective has focused on the H protein, which the virus uses to bind to human cells, a key step in viral replication. Our bodies can produce eight different antibodies that each recognize a different part of the H protein. Scientists studied measles viruses that carried mutations that disrupted each of these eight locations on the H protein in different combinations. They discovered through laboratory tests that carrying a mutation that makes the virus unrecognizable to one antibody was not enough to give the virus an advantage over our immune defenses. Even carrying several mutations was not helpful. To get a leg up in the lab trials, the mutant viruses needed to have five or more mutations in the H protein, something with a vanishingly small chance of occurring through random mutation out in the real world. The researchers also found that all those mutations come with a downside: some of them make the H protein unable to do its job. A virus lucky enough to acquire the right mutations and escape immune detection in a vaccinated person would likely find itself unable to attach to a human cell to start the process of replication. Furthermore, antibodies against the F protein, the other surface protein in measles, would still be able to tamp down the infection.
Even though the measles virus churns out a wide variety of new mutants as it multiplies, it seems to be nearly impossible for measles to evolve in a way that lets it both evade the immune defenses that vaccination provides and maintain its ability to replicate and spread. This stands in contrast to, for example, the flu virus, in which a single mutation can provide a big advantage in terms of escaping detection by the human immune system.
While the viruses that cause measles, COVID-19, the flu, and HIV all have RNA genomes and high mutation rates, the vaccine outlook for measles is markedly different from that of the other three diseases. All of science’s substantial efforts towards developing an HIV vaccine have so far been disappointingly unsuccessful. The influenza vaccine is 30-60% effective, an important boost in preventing a pandemic, but needs to be reformulated and readministered every year. The COVID-19 vaccines reduce the risk of life-threatening illness by 70%, but this effect wanes over time, and boosters and reformulations of the vaccine are required. In comparison, the measles vaccine, usually received in the form of the MMR shots, is a standout. It is 97% effective at preventing the disease, provides life-long immunity with just two doses, and never needs updating. Add to that 50+ years of data and experience backing up its safety, and there’s no question that the MMR vaccine is a critical tool to protect public health in general and children’s lives in particular. Now all we need to do is use it.
Primary literature:
- Muñoz-Alía, M. Á., Nace, R. A., Zhang, L., and Russell, S.J. (2021). Serotypic evolution of measles virus is constrained by multiple co-dominant B cell epitopes on its surface glycoproteins. Cell Reports Medicine. 2: 100225. Read it »
News articles:
- A report on the current measles outbreak from NBC
- A quick summary of the 2021 research on constraints on measles virus evolution from the Mayo Clinic
- A handy explanation for why some vaccines work better than others from the American Society for Microbiology
Understanding Evolution resources:
- In your own words, explain what a mutation is.
- According to the article above, what two differences between RNA and DNA are responsible for their different mutation rates?
- What key similarity might lead us to expect that the viruses behind measles, HIV, flu, and COVID-19 would all have high rates of evolution?
- Why does rapid viral evolution present a challenge for vaccine development?
- Review this webpage that describes three limitations on natural selection’s power to produce adaptive evolutionary change.
- The news article above describes research showing that the measles virus would need to have five or more mutations to achieve an advantage over an immune system primed by vaccination. To which of the three limitations on natural selection does this correspond? Explain your reasoning
- The news article above also describes how mutations that would help the virus escape detection by a vaccine-primed immune system affect the function of the H protein. To which of the three limitations on natural selection does this correspond? Explain your reasoning
- Teach about the causes of mutation: In this article (and the linked assignments and student readings) for the college level, students examine and interpret data that scientists use to study the causes of mutations that matter most for evolution. Use the tabs at the bottom of the feature to find related videos, assignments, and lessons to build this example into a lesson sequence on mutation.
- Teach about variation and natural selection: This short film and exercise for grades 9-12 reinforce the concepts of variation and natural selection using the rock pocket mouse system.
- Teach about viral evolution and vaccines: This news story for high school and college students connects the concept of an evolutionary arms race to vaccines. Discussion questions are included.
- Bankamp, B., Takeda, M., Zhang, Y., and Rota, P. A. (2011). Genetic characterization of measles vaccine strains. The Journal of Infectious Diseases. 204: S533–48.
- Centers for Disease Control and Prevention. (May 9, 2024). Measles symptoms and complications. CDC. Retrieved February 26, 2025, from the CDC (https://www.cdc.gov/measles/signs-symptoms/index.html).
- Centers for Disease Control and Prevention. (May 29, 2024). About measles. CDC. Retrieved February 26, 2025, from the CDC (https://www.cdc.gov/measles/about/index.html).
- Centers for Disease Control and Prevention. (August 14, 2024). CDC seasonal flu vaccine effectiveness studies. CDC. Retrieved February 26, 2025, from the CDC (https://www.cdc.gov/flu-vaccines-work/php/effectiveness-studies/index.html).
- Centers for Disease Control and Prevention. (January 13, 2025). Benefits of getting vaccinated. CDC. Retrieved February 26, 2025, from the CDC (https://www.cdc.gov/covid/vaccines/benefits.html).
- Greaney, A. J., Welsh, F. C., and Bloom, J. D. (2021). Co-dominant neutralizing epitopes make anti-measles immunity resistant to viral evolution. Cell Reports Medicine. 2: 100257.
- Kwai, I. (February 22, 2025). Measles outbreaks in Texas and New Mexico sicken nearly 100 people. The New York Times. Retrieved February 26, 2025, from the New York Times (https://www.nytimes.com/2025/02/22/us/texas-measles-outbreak.html).
- Lee, J. M., Eguia, R., Zost, S. J., Choudhary, S., Wilson, P. C., Bedford, T., … and Bloom, J. D. (2019) Mapping person-to-person variation in viral mutations that escape polyclonal serum targeting influenza hemagglutinin. eLife. 8: e49324.
- Muñoz-Alía, M. Á., Nace, R. A., Zhang, L., and Russell, S.J. (2021). Serotypic evolution of measles virus is constrained by multiple co-dominant B cell epitopes on its surface glycoproteins. Cell Reports Medicine. 2: 100225.
- Ng'uni, T., Chasara, C., and Ndhlovu, Z. M. (2020). Major scientific hurdles in HIV vaccine development: historical perspective and future directions. Frontiers in Immunology. 11: 590780.
- Sanjuán, R., Nebot, M. R., Chirico, N., Mansky, L. M., and Belshaw, R. (2010). Viral mutation rates. Journal of Virology. 84: 9733-48.
- World Health Organization. (December 5, 2019). More than 140,000 die from measles as cases surge worldwide. World Health Organization New. Retrieved February 26, 2025, from the World Health Organization (https://www.who.int/news/item/05-12-2019-more-than-140-000-die-from-measles-as-cases-surge-worldwide).
- World Health Organization. (November 14, 2024). Measles. World Health Organization Newsroom. Retrieved February 26, 2025, from the World Health Organization (https://www.who.int/news-room/fact-sheets/detail/measles).