Only a few decades ago, antibiotics were considered to be wonder drugs because they worked so well to cure deadly diseases. Ironically, though, many antibiotics have become less effective, precisely because they have worked so well and have been used so often.
Making inroads against infectious disease
The antibiotic era began in 1929 with Alexander Fleming’s observation that bacteria would not grow near colonies of the mold Penicillium. In the decades that followed this breakthrough discovery, molecules produced by fungi and bacteria have been successfully used to combat bacterial diseases such as tuberculosis and pneumonia. Antibiotics drastically reduced death rates associated with many infectious diseases.
Infectious diseases strike back
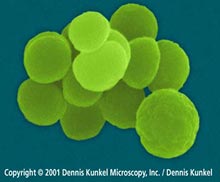 The golden age of antibiotics proved to be a short-lived one. During the past few decades, many strains of bacteria have evolved resistance to antibiotics. An example of this is Neisseria gonorrhoeae, the bacteria that causes gonorrhea, shown at right. In the 1960s penicillin and ampicillin were able to control most cases of gonorrhea. Today, more than 24 percent of gonorrheal bacteria in the U.S. are resistant to at least one antibiotic, and 98 percent of gonorrheal bacteria in Southeast Asia are resistant to penicillin.1 Infectious bacteria are much harder to control than their predecessors were ten or twenty years ago.
The golden age of antibiotics proved to be a short-lived one. During the past few decades, many strains of bacteria have evolved resistance to antibiotics. An example of this is Neisseria gonorrhoeae, the bacteria that causes gonorrhea, shown at right. In the 1960s penicillin and ampicillin were able to control most cases of gonorrhea. Today, more than 24 percent of gonorrheal bacteria in the U.S. are resistant to at least one antibiotic, and 98 percent of gonorrheal bacteria in Southeast Asia are resistant to penicillin.1 Infectious bacteria are much harder to control than their predecessors were ten or twenty years ago.
Doctors miss the “good old days,” when the antibiotics they prescribed consistently cured their patients. However, evolutionary theory suggests some specific tactics to help slow the rate at which bacteria become resistant to our drugs.
Applying our knowledge of evolution
Evolutionary theory predicted that bacterial resistance would happen. Given time, heredity, and variation, any living organisms (including bacteria) will evolve when a selective pressure (like an antibiotic) is introduced. But evolutionary theory also gives doctors and patients some specific strategies for delaying even more widespread evolution of antibiotic resistance. These strategies include:
- Don’t use antibiotics to treat viral infections.
Antibiotics kill bacteria, not viruses. If you take antibiotics for a viral infection (like a cold or the flu), you will not kill the viruses, but you will introduce a selective pressure on bacteria in your body, inadvertently selecting for antibiotic-resistant bacteria. Basically, you want your bacteria to be “antibiotic virgins,” so that if they someday get out of hand and cause an infection that your immune system can’t handle, they can be killed by a readily available antibiotic.  Avoid mild doses of antibiotics over long time periods.
Avoid mild doses of antibiotics over long time periods.
If an infection needs to be controlled with antibiotics, a short-term, high-dosage prescription is preferable. This is because you want to kill all of the illness-causing bacteria, leaving no bacterial survivors. Any bacteria that survive a mild dose are likely to be somewhat resistant. Basically, if you are going to introduce a selective pressure (antibiotics), make it so strong that you cause the extinction of the illness-causing bacteria in the host and not their evolution into resistant forms.- When treating a bacterial infection with antibiotics, take all your pills.
Just as mild doses can breed resistance, an incomplete regimen of antibiotics can let bacteria survive and adapt. If you are going to introduce a selective pressure (antibiotics), make it a really strong one and a long enough one to cause the extinction of the illness-causing bacteria and not their evolution. - Use a combination of drugs to treat a bacterial infection.
If one particular drug doesn’t help with a bacterial infection, you may be dealing with a resistant strain. Giving a stronger dose of the same antibiotic just increases the strength of the same selective pressure — and may even cause the evolution of a “super-resistant” strain. Instead, you might want to try an entirely different antibiotic that the bacteria have never encountered before. This new and different selective pressure might do a better job of causing their extinction, not their evolution. - Reduce or eliminate the “preventive” use of antibiotics on livestock and crops.
Unnecessary use of antibiotics for agricultural and livestock purposes may lead to the evolution of resistant strains. Later, these strains will not be able to be controlled by antibiotics when it really is necessary. Preventive use of antibiotics on livestock and crops can also introduce antibiotics into the bodies of the humans who eat them.
Ultimately, recognizing bacteria as evolving entities and understanding their evolution should help us to control that evolution, allowing us to prolong the useful lifespan of antibiotics.